US researchers working with pigs discovered a way of lowering appetite as effectively as
bariatric surgery except they used minimally invasive surgery that suppresses the
hunger hormone ghrelin by vaporizing the main blood vessel that carries blood to the top section of the stomach (the fundus). The study was the work of researchers at Johns Hopkins Medical Institutions in Baltimore, Maryland, and the School of Veterinary Medicine, University of Pennsylvania, Philadelphia, and is published in the October 1st issue of Radiology.
The researchers wrote that about 90 per cent of the body's ghrelin comes from the fundus, and it needs a good blood supply to make it.
First author Dr Aravind Arepally said:
"With gastric artery chemical embolization, called GACE, there's no major surgery."
"In our study in pigs, this procedure produced an effect similar to bariatric surgery by suppressing ghrelin levels and subsequently lowering appetite," added Arepally, who is clinical director of the Center for Bioengineering Innovation and Design and associate professor of radiology and surgery at the John Hopkins University School of Medicine.
Arepally and colleagues wrote that the last ten years have seen several unsuccessful attempts to suppress grehlin safely and easily.
Bariatric surgery is where part of the stomach or bowel is either removed, reconstructed or bypassed. It suppresses appetite and results in significant weight loss. However, there are significant risks because it is an invasive and complex procedure.
Arepally explained that:
"Obesity is the biggest biomedical problem in the country, and a minimally invasive alternative would make an enormous difference in choices and outcomes for obese people."
For the study, Arepally and colleagues worked with 10 healthy and growing pigs for 4 weeks. Pigs were chosen because they their bodies have similar anatomy and physiology to humans. Baseline readings for ghrelin and other measures were obtained by fasting the pigs overnight, weighing them and taking blood samples.
The pigs were then put into two groups, one for the treatment and the other was the control group. Both groups underwent a procedure that used X rays to guide the surgery where researchers inserted a thin tube in the large blood vessel near the groin and then into the left gastric arteries supplying blood to the stomach.
In the treatment group (GACE group) they injected the site once with sodium morrhuate, a chemical that destroys blood vessels, and in the control group they injected the site once with saline.
The researchers monitored the blood levels of ghrelin for 4 weeks.
The results showed that:
Changes in ghrelin levels over time were significantly different between control and GACE treated pigs (P < .004). In the GACE treated pigs, the levels of ghrelin were suppressed by as much as 60 per cent compared to baseline levels. The percentage change in ghrelin levels in GACE treated pigs went down from baseline to -34, -38.6, -42.5, and -12.9 per cent during weeks 1 to 4, respectively. In the control pigs, the percentage change in ghrelin was -1.7, -9.7, +2.6, and +18.2 per cent during weeks 1 to 4, respectively. At the end of 4 weeks, the control pigs continued to gain weight, putting on 15.1 per cent their original weight in that time, while the GACE pigs' weight plateaued at an increase of 7.8 per cent from their original weight.
The authors concluded that: "Catheter-directed GACE can suppress the appetite hormone ghrelin and affect weight gain." Arepally said appetite is not an easy process to understand or control because it involves both the body and the mind. Ghrelin levels go up and down throughout the day, and they respond to emotional as well as physiological circumstances. "But", Arepally pointed out, "even if the brain says 'produce more ghrelin', GACE physically prevents the stomach from making the hunger hormone".
Source:
Medical News Today
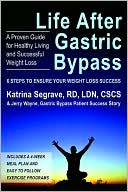
 Losing weight may help resolve erectile dysfunction in obese men, according to research presented today at the 103rd Annual Scientific Meeting of the American Urological Association (AUA). Morbid obesity can cause sexual dysfunction independent of other common confounders, including diabetes, hypertension and smoking. In this study from researchers in Boston and Philadelphia, sexual function was normalized in some men who underwent gastric bypass surgery for weight loss.
Losing weight may help resolve erectile dysfunction in obese men, according to research presented today at the 103rd Annual Scientific Meeting of the American Urological Association (AUA). Morbid obesity can cause sexual dysfunction independent of other common confounders, including diabetes, hypertension and smoking. In this study from researchers in Boston and Philadelphia, sexual function was normalized in some men who underwent gastric bypass surgery for weight loss.